Australian Bushfires Worsen Rural Mental Health Crisis
The 2019-20 bushfire season has been catastrophic, and there is no clear end in sight. So far, 4 people have lost their lives, over 400 homes have been destroyed and countless pets and wildlife have perished. Even as residents slowly return to their homes or communities, many adults and children will continue to experience poor mental health due to sheer loss and grief.
Unfortunately, traumatic natural disasters are far too common for Australia's rural and remote dwellers, many of whom rely solely on their crops and livestock for income.
In addition to these severe environmental conditions, rural and remote Australians tend to have fewer job opportunities, lower incomes and stronger negative stigmas about mental health. These factors combined, along with the geographical isolation and lack of access to mental healthcare professionals, make it easy to see why there is a mental health crisis in the Aussie bush.
- Rural and remote dwellers are 1.8 times more likely to be hospitalised for intentional self-harm, and 2.2 times more likely to die by suicide -
PM Scott Morrison has acknowledged that our current suicide prevention strategies are failing and that changes must be made. He recently appointed a new suicide prevention adviser, Christine Morgan, to assess Australia’s current suicide prevention strategies.
She has been advised to return in 18 months with future recommendations, to completely overhaul our current system. Given the Health Minister's support for telehealth services as a future proof healthcare delivery option, we are confident that digital strategies, such as telehealth, will also be included in Christine's recommendations.
Telehealth video consultations or text sessions are particularly effective in rural and remote areas due to their ability to break down the barrier of distance and avoid negative stigmas. Patients can have private sessions with licensed professionals from the comfort of their own home. They can also save both time and money that would otherwise be used for travelling to and from the practitioner's office.
The CEO of the American Telemedicine Association, Ann Mond Johnson, highlighted that video consultations, particularly those for mental health services, often compel the patient and provider to actually look each other in the eye. She also explains that telehealth improves interactions for patients that are uncomfortable seeing healthcare providers in person. The existence of a screen or ‘barrier’ between both parties can encourage the patient to be more honest and forthcoming about issues or concerns that they may have. This, in turn, improves patient health outcomes.
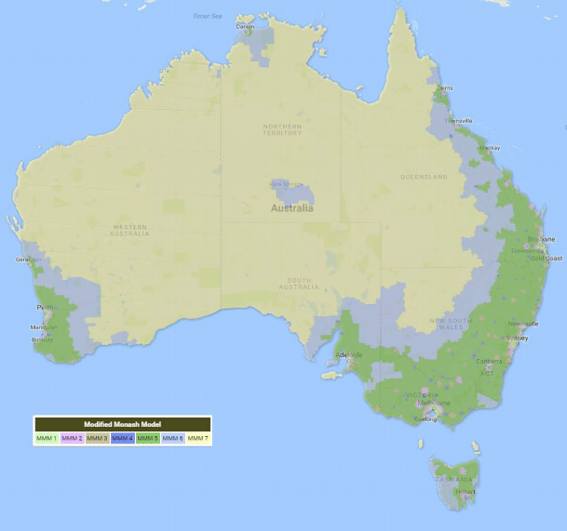
There are also numerous telehealth rebates for mental health treatment, particularly for rural and remote Australians located in Modified Monash Model areas 3-7.
GP's can provide care under the Drought Communities Scheme and the Better Access Scheme. Psychiatrists can also access rebates, as can psychologists, social workers and occupational therapists.
If you are interested in using telehealth in your practice, click here.
If you are a patient and would like to find a mental health care provider, click here.
For more information about how to donate and help with the bushfires, click here.




