Dr Silvia Pfeiffer Speaks at the National Telehealth Summit
On 20th April, Coviu CEO and Co-founder, Dr Silvia Pfeiffer, joined other industry experts to present at the National Telehealth Summit at the Swissôtel Sydney.
This is a transcript of her presentation on New Models of Care and the Financial Opportunities for Healthcare Businesses .
'Welcome everyone to my talk about opportunities that telehealth is offering in primary care.
I’m Silvia Pfeiffer and I’m the CEO of Coviu, a custom-built secure telehealth platform that was created as a spinout from the CSIRO in 2018.
My background is in technology, but I’ve worked with providers across Allied Health and General Practice since 2012 to create a platform that really helps them with the uptake of video telehealth.
I’d like to specifically focus on video telehealth. Video is the digital innovation that is coming to Primary Care, seeing as the phone has been around for 150 years and isn’t really providing us any new ways of delivering care.
At Coviu, we've enabled the delivery of over 3 million video consultations in 2020. All of these have been delivered by clinicians to their own patients. We strongly believe in continuity of care and development of a trusted relationship of patients with their local providers.
It is important to put patients’ needs at the centre of a health consultation. The introduction of Medicare items for video telehealth has opened up the eyes of urban patients as to what is possible and has created persistent change for rural patients.
So let’s look at the opportunities for patients first.
Telehealth has allowed delivering care to patients that would otherwise miss out - be that people in rural areas, older citizens that cannot find a family member to take them to a practitioner, or a person suffering from mental health that cannot leave their home.
In mental health, practitioners have actually found that video telehealth offers them an opportunity to better understand a patient’s background just by looking into their home. As an image provides more information than 1000 words, a video provides more information than 100,000 words!
We’ve also seen that busy professionals who never find the time to see their clinician have been able to fit in online visits more easily thus allowing the detection of issues earlier than via an in-person visit.
And finally, many patients have been ecstatic to learn that they can see their family doctor via a video call during the pandemic without having to pull a sick child out of their bed and manage the supervision of the other children.
So, we know that patients are excited about the opportunities of video telehealth. But clinicians have also embraced it as new opportunities for a more flexible work environment.
Clinicians have been able to offer out-of-hours services from their homes.
Clinicians have been able to move to part-time online care to allow them to better integrate family and work life.
Clinicians have been able to move to different locations but continue to offer services to their prior patients with whom they had built great relationships. They would simply associate with their GP practice as a remote provider.
There are real opportunities for healthcare practices to their bottom line in delivering video telehealth so let me just talk about money for a moment.
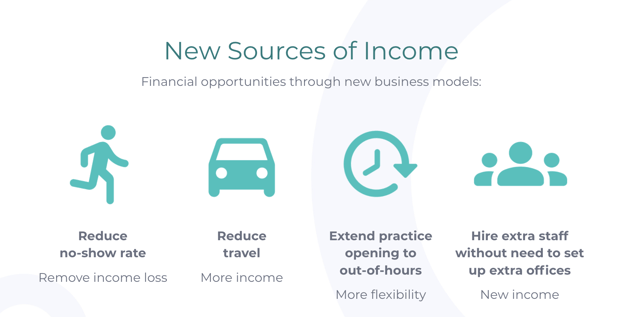
Financial advantages for practices come come from:
- a reduction of the no-show rate
- a reduction of travels to patients
- an ability to offer extended practice hours without hiring more practice staff
- an ability to hire more clinicians without having to extend the number of staff and offices in your practice
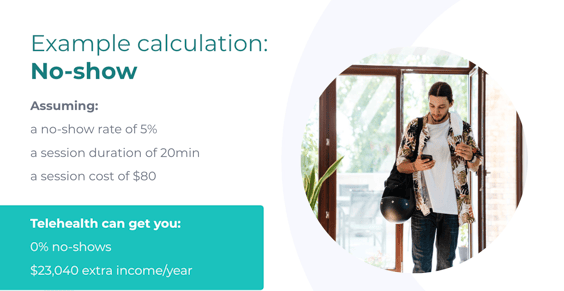
Here are just some monetary examples that show you potential financial impact:
- For a practice with a no-show rate of 5%, you can create $20-$25K extra income per clinician as that no-show rate tends towards 0 on video telehealth
- For a practice where clinicians need to travel 10 hours a week, telehealth can create a similar extra income of $25-$30k a year per clinician
- An extension of opening hours by 2 hours a day can similarly create an addition $25-$30k annually per clinician
But there are new models of care that extend beyond the direct monetary impact. Here are just three ideas:
- Creating integrated care offerings that go beyond one-off care touch points
- Creating shared care planning opportunities with other specialists and the whole care team of the patient
- An opportunity to extend access to the data that patients capture about themselves that give clinicians more information about their health
What we should change in primary care is the modalities through which they a patient can communicate with their clinician.
We have heard a lot of frustration by patients that their usual GP is not offering video telehealth any more, so patient choice is being limited by their practitioner despite having patient demand.
It will be important to understand that patients will vote with their feet. We have already seen patients leave practices that don’t offer telehealth in favour of ones that do.
Let’s embrace the opportunities in front of us and start offering services in the way that patients want.'
To learn more about how telehealth can work for your practice, chat to a telehealth expert today.
.png?width=460&name=Untitled%20design%20(18).png)



)%20(Presentation%20(169))%20(22)-2.png)